Sleep in the Long-Term Care Setting
By Mary Jo Vetter, and Patrick Luib
Sleep is a restorative physiologic process that is essential for maintaining health. High-quality sleep is necessary for optimal cognitive and physical functioning, especially for residents living with a disease that causes cognitive impairment such as dementia.
While some sleep disturbances are part of the normal aging process, sleep fragmentation can increase as dementia progresses. Some of the most common physiological concerns associated with poor sleep include a weaker immune system, psychomotor performance challenges such as loss of balance, increased pain sensitivity, and changes to the metabolic and endocrine systems.
The importance of sleep may not be well understood in the nursing home industry as a clinical matter directly relating to a resident’s health and quality of life, and bedside staff may not understand their role in promoting high-quality sleep.
Compared to community-dwelling older adults, those living in long-term care (LTC) facilities, on average, experience up to 2 hours of nighttime wakefulness and have symptoms of insomnia that contribute to daytime sleepiness and fatigue resulting in an increased incidence of falls, cognitive decline, depression, and poor quality of life (Kim & Yoon, 2020).
LTC residents typically have a multimorbid clinical profile encompassing advanced chronic diseases, functional impairments, and mental health issues that contribute to sleep and circadian rhythm disturbances. These risk factors, combined with psychosocial and environmental issues associated with the care setting, lead to an increased vulnerability that perpetuate sleep disturbances.
Contributing elements, such as reduced daytime activity, excessive daytime napping, and poor sleep hygiene, affect sleep negatively.
Some residents are affected by a non-stimulating environment, are mainly sedentary during the day, and do not spend sufficient time communicating with others or engaging in leisure activities.
Others may encounter an over-stimulating nighttime environment due to light and noise of facility operations and staff routines related to incontinence care, pain management, or disruptive behavior such as agitation, aggression, or wandering (Capezuti et al., 2018).
Sleep disturbances often lead to providers prescribing psychoactive medications, which are associated with negative adverse effects and further impact sleep quality.
Non-pharmacologic management of poor sleep in the LTC facility should be a primary intervention and consists of a multidimensional approach targeted to both the individual and systems level of care (Morley, 2015).
DREAM Toolkit
In February 2020, the Centers for Medicare & Medicaid Services (CMS) released the Developing a Restful Environment Action Manual (DREAM) toolkit (U.S. Department of Health and Human Services, 2020).
This toolkit offers education and person-centered, practical interventions that nursing home administrators, directors of nursing, and bedside staff can implement to promote high-quality sleep for residents living with dementia.
DREAM consists of an Implementation Guide, Handbook, Sleep Matters Video, Pocket Guide for Clinical Teams, Sleep Environment Improvement Tool, and Resident Preferences Tool. All components are available on the download section of CMS’ CMPRP webpage, including Sleep Matters Video.
The foundation of this toolkit is based on the work of a Technical Expert Panel chaired by Alice Bonner. The panel established a driver diagram that was iterated upon by a Dementia Care Breakthrough Community of approximately 30 nursing homes across the country.
Leaders and front-line staff in each facility participated in three learning sessions including action periods where rapid cycles of improvement were used to test several change ideas.
The Breakthrough Community identified best practices in sleep hygiene techniques to improve residents’ sleep and quality of life. Figure 1 describes each component and respective nursing home staff.
Figure 1. Who Can Use the Toolkit?
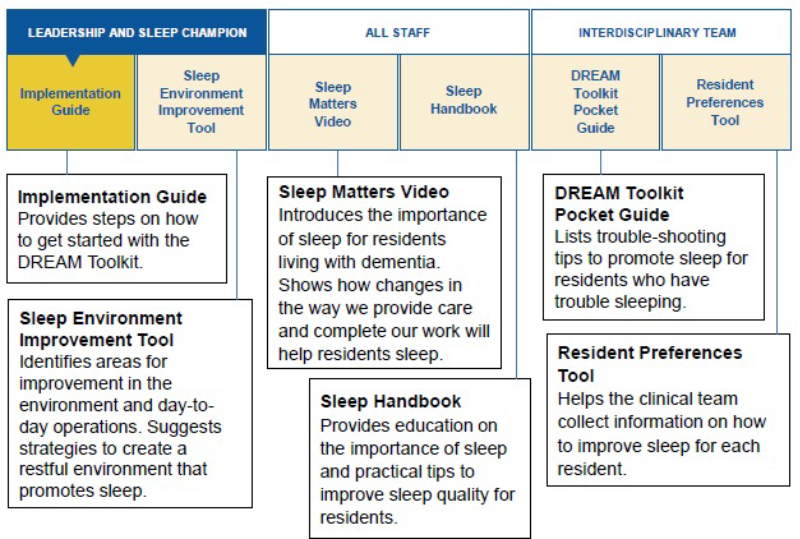
The Implementation Guide informs nursing leaders why sleep is important and identifies tips to sustain progress and overcome potential barriers.
The Handbook offers visual education material on the importance of sleep and includes strategies to improve sleep quality for residents, which can be used as a series of one-pagers. Sleep Environment Improvement Tool identifies approaches to creating a restful environment in the nursing home to promote sleep.
For example, suggested approaches for issues concerning adequate lighting include creating a schedule to turn common area lights off and on. The third component is a Pocket Guide, which provides reminders on strategies to promote sleep.
Resident Preferences Tool is the fourth component and includes questions staff can ask residents to learn more about their sleep preferences and create individualized bedtime routines.
The Sleep Matters Video explains the importance of sleep for residents living with dementia.
Multiple physical, psychosocial, and environmental factors have an impact on sleep among older adults in LTC facilities. While aging and underlying disease processes impact sleep quality, there is a reciprocal relationship between an individual’s health status and controllable factors in the environment.
Geared at decreasing exacerbation of sleep issues, the DREAM Toolkit provides non-pharmacological interventions to improve nursing home sleep environments and person-centered approaches to support the highest-quality sleep for each resident.
Mary Jo Vetter, DNP, AGPCNP-BC
mjv5@nyu.edu
Patrick Luib, APRN, BC, MSN
patrick.luib@gmail.com
References
Capezuti, E., Zadeh, R., Pain, K., Basara, N.Z., & Kreiger, A. (2018). A systematic review of non-pharmacological interventions to improve nighttime sleep among residents of long-term care settings. BMS Geriatrics, 18, Article No. 143. https://doi.org/10.1186/s12877-018-0794-3
Kim, D.E., & Yoon, J.Y. (2020). Factors that influence sleep among residents in long-term care facilities. International Journal of Environmental Research and Public Health, 17(6), 1889. https://doi.org/10.3390/ijerph17061889
Morley, J. (2015). Sleep and the nursing home. Journal of the American Medical Directors Association, 16(7), 539-543. https://doi.org/10.1016/j.jamda.2015.05.001
U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. (2020). Release of additional toolkits to ensure safety and quality in nursing homes. https://www.cms.gov/files/document/qso-20-11-nh.pdf